Weighted Blankets for Dementia Improve Sleep and Reduce Anxiety
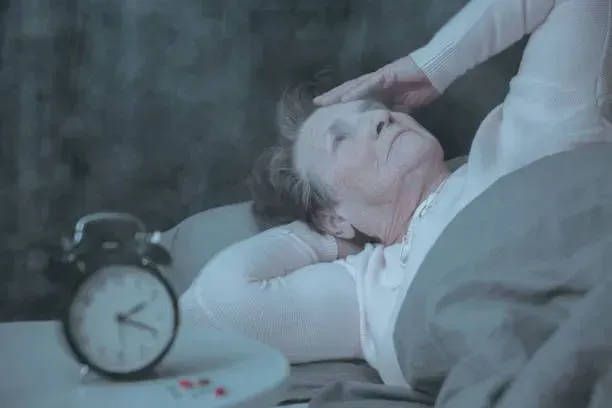
As the prevalence of dementia continues to rise, the importance of exploring non-pharmacological interventions to improve the quality of life for individuals with dementia becomes increasingly evident. One such promising approach gaining recognition is the use of weighted blankets. These blankets, designed to provide gentle pressure evenly distributed across the body, have shown remarkable potential in improving sleep and reducing anxiety among individuals living with dementia.
The Challenge of Sleep Disturbances and Anxiety in Dementia:
Dementia often brings with it a host of challenges, among which sleep disturbances and heightened anxiety are prevalent. According to the Alzheimer's Association, sleep disturbances affect up to 40% of individuals with Alzheimer's disease, leading to increased caregiver burden and a decline in overall well-being. Statistics indicate that anxiety symptoms are prevalent in about 25% to 70% of individuals with dementia, adding an additional layer of complexity to their daily lives.
Individuals with dementia often face a myriad of challenges, with sleep disturbances and heightened anxiety standing out as particularly pervasive and impactful issues. Sleep disturbances in dementia are a complex and multifaceted phenomenon, affecting both the quantity and quality of sleep - manifesting as difficulties falling asleep, frequent waking during the night, or a tendency to wake up early in the morning. These disturbances not only compromise the overall well-being of individuals with dementia but also contribute to an increased burden on caregivers who often grapple with the challenges of providing care to someone with erratic sleep patterns.
In addition to sleep disturbances, anxiety is a prevalent and often under-recognized symptom in individuals with dementia, intensifying the complexity of their cognitive and emotional experience. Anxiety in dementia can manifest in various forms, including restlessness, repetitive behaviors, and verbal expressions of distress. The interplay between anxiety and cognitive decline further exacerbates the challenges of dementia care, as heightened anxiety can contribute to a decline in overall functioning and further compromise the quality of life for both individuals with dementia and their caregivers. Addressing these intertwined challenges requires a comprehensive and tailored approach that considers the unique needs of each individual within the context of dementia care. It is in this context that the use of weighted blankets emerges as a promising intervention to address some of these challenges.
The Science Behind Weighted Blankets:
Weighted blankets operate on the principle of Deep Touch Pressure (DTP), a therapeutic technique that applies gentle pressure to the body, promoting a sense of security and relaxation. This pressure has been found to stimulate the release of neurotransmitters like serotonin and dopamine, promoting a calming effect on the nervous system. Deep Touch Pressure (DTP) therapy, which underlies the use of weighted blankets, has its origins in various therapeutic practices that involve the application of gentle pressure to the body. One of the earliest and most well-known forms of DTP is deep pressure stimulation, which has roots in occupational therapy and sensory integration techniques.
The concept of deep pressure stimulation can be traced back to the work of occupational therapist and pioneer in sensory integration theory, Dr. Jean Ayres. In the 1960s, Dr. Ayres developed the theory of sensory integration, which focuses on how the brain processes and organizes sensory information from the body and the environment. According to this theory, individuals with sensory processing disorders may have difficulty organizing and responding to sensory input, leading to challenges in daily functioning.
Deep pressure stimulation, as part of sensory integration therapy, involves the application of pressure to the body to help individuals regulate and process sensory information more effectively. This pressure can be delivered through various means, including massage, compression garments, and, more recently, weighted items such as blankets.
The use of weighted blankets specifically as a form of deep touch pressure therapy gained popularity in the late 1990s and early 2000s. Occupational therapists and researchers began exploring the benefits of using weighted blankets, particularly for individuals with sensory processing disorders, anxiety, and certain neurological conditions. The idea is that the evenly distributed weight of the blanket provides a calming and organizing effect on the sensory system.
While the roots of deep touch therapy can be traced to sensory integration theory, its application has expanded beyond the realm of sensory processing disorders. Today, deep touch therapy, particularly in the form of weighted blankets, is utilized in various contexts, including anxiety management, stress reduction, and sleep improvement for individuals with conditions such as insomnia and certain neurological disorders.
Studies Supporting the Efficacy of Weighted Blankets:
A comprehensive review of studies reveals a growing body of evidence supporting the use of weighted blankets for individuals with dementia. A study published in the Journal of Sleep Medicine & Disorders found that individuals using weighted blankets experienced improved sleep quality, with 63% reporting reduced insomnia symptoms.
Furthermore, a randomized controlled trial conducted by the Journal of Medical Internet Research demonstrated that the use of weighted blankets significantly reduced anxiety levels in individuals with dementia compared to a control group. These findings underscore the potential of weighted blankets as a non-invasive and cost-effective tool in managing sleep disturbances and anxiety in dementia.
Practical Considerations and Recommendations:
While the evidence supporting the use of weighted blankets for dementia is promising, it is crucial to approach their implementation with careful consideration. Before introducing a weighted blanket, consultation with a healthcare professional is advisable to ensure its appropriateness for the individual's specific health condition.
Additionally, selecting an appropriately weighted blanket is essential, with recommendations suggesting a weight equivalent to about 10% of the individual's body weight. Proper supervision and regular monitoring are also key to ensuring the continued effectiveness and safety of this intervention.
In the realm of dementia care, where the search for effective, non-pharmacological interventions is ongoing, weighted blankets stand out as a simple yet impactful tool. The evidence supports their role in improving sleep and reducing anxiety in individuals with dementia. As 7 Day Home Care continues to provide specialized Alzheimer's and dementia in-home care in Queens, Manhattan, Brooklyn, Nassau County, and Suffolk County, New York, we have seen the integration of weighted become a valuable component to a holistic approach to dementia care. Through ongoing research and practical application, we aim to contribute to the growing body of knowledge that seeks to enhance the well-being of individuals living with dementia. Contact 7 Day Home Care at 516-408-0034 today to learn more about our specialized Alzheimer's and Dementia Care, Person-Centered Home Care, and Patient-Caregiver Matching Methodology.
Brian Callahan
7 Day Home Care










